Welcome back to another adventure along The Hitchhiker’s Guide to Medicine! Today, we look at a study discussing menopause and its relation to a decline in cognitive health.
Menopause is a significant biological transition in a woman’s life, marked by the cessation of menstrual cycles and a decline in estrogen levels. While its impact on reproductive health is well-documented, researchers are increasingly uncovering its role in cognitive function and brain aging. A new study highlights a potential link between menopause symptoms—particularly sleep disturbances, depression, and vasomotor symptoms (hot flashes and night sweats)—and an increased risk of future memory and cognitive decline.
This growing body of evidence underscores the need to recognize menopause as not just a hormonal shift but a phase with profound neurological implications. Let’s explore how menopause symptoms may serve as early indicators of cognitive issues and what women can do to support brain health during this transition.
Menopause leads to a sharp decline in estrogen, a hormone that plays a crucial role in brain function. Estrogen supports neurotransmitter activity, reduces inflammation, and promotes blood flow to the brain. The loss of estrogen during menopause is associated with changes in brain metabolism, reduced connectivity in memory-related regions, and increased susceptibility to neurodegenerative diseases like Alzheimer’s.
One of the most common complaints during menopause is poor sleep, often due to night sweats and insomnia. Sleep is essential for memory consolidation and brain detoxification, processes that occur during deep sleep phases. Disruptions in sleep architecture can impair attention, processing speed, and long-term memory formation. Chronic sleep deprivation is also associated with the buildup of beta-amyloid, a protein linked to Alzheimer’s disease.
Depression and anxiety frequently accompany menopause, often as a result of fluctuating hormone levels. Research suggests that mood disorders can accelerate brain aging, impairing hippocampal function—the region responsible for memory and learning. Chronic stress and depression also increase levels of cortisol, a hormone that, in excess, can shrink brain volume and weaken neural connectivity.
Vasomotor symptoms like hot flashes and night sweats are more than just a nuisance. Studies using brain imaging techniques have shown that frequent hot flashes are linked to reduced gray matter volume in areas associated with memory and cognition. Some researchers propose that hot flashes reflect underlying instability in the brain’s thermoregulatory centers, which may also signal broader disruptions in neural function.
The findings from this recent study suggest that menopause symptoms could be early warning signs of cognitive decline. Women with severe or persistent menopause symptoms may have a higher risk of developing mild cognitive impairment (MCI), a precursor to Alzheimer’s and other dementias.
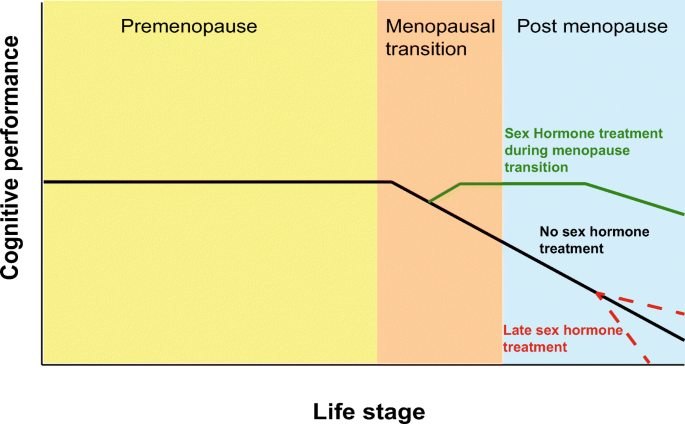
While not all women experience significant cognitive issues during menopause, those with intense symptoms should be particularly mindful of brain health. Longitudinal studies suggest that early intervention—such as hormone therapy, lifestyle changes, and cognitive exercises—may help mitigate risks.
Although menopause-related cognitive changes can be concerning, proactive strategies can help support brain health during this transition:
- Prioritize Sleep Hygiene – Maintaining a consistent sleep schedule, avoiding blue light exposure before bedtime, and using relaxation techniques can improve sleep quality.
- Manage Stress and Mood – Practices like mindfulness meditation, yoga, and cognitive-behavioral therapy (CBT) can help regulate mood and reduce cortisol levels.
- Consider Hormone Therapy – Estrogen replacement therapy (ERT) has been shown to have potential cognitive benefits, particularly when initiated early in menopause. However, it is not suitable for all women, and risks should be discussed with a healthcare provider.
- Adopt a Brain-Healthy Diet – Diets rich in antioxidants, omega-3 fatty acids, and plant-based nutrients—such as the Mediterranean diet—can help protect against neurodegeneration.
- Stay Physically Active – Exercise improves blood flow to the brain, reduces inflammation, and enhances neuroplasticity, supporting cognitive resilience.
- Engage in Mental Stimulation – Activities such as reading, puzzles, learning new skills, and social interactions can strengthen neural pathways and delay cognitive decline.
Menopause is often viewed through the lens of reproductive aging, but its effects on cognitive health are equally important. As research continues to uncover the links between menopause symptoms and future memory issues, it becomes clear that addressing these symptoms is not just about improving quality of life—it’s about safeguarding long-term brain health.
Women experiencing significant menopause symptoms should seek medical advice and adopt proactive strategies to support cognitive function. By recognizing menopause as a critical period for brain health, we can move toward a more comprehensive approach to aging that prioritizes both physical and cognitive well-being.
Stay tuned to “The Hitchhiker’s Guide to Medicine” as we uncover more marvels and milestones in the field of medical science. Until then, keep exploring, and stay curious!

Leave a comment